Intensive Care on the Fly
DHART Marks 30 Years of Transforming Critical Care
By 7:00 am on July 1, 1994, the new air medical transport program at Dartmouth Hitchcock Medical Center (DHMC) was finally ready to take off. Seven minutes later, the helicopter program got its first call—far sooner than Norm Yanofsky, MD, expected.
“We didn’t have high expectations,” says Yanofsky, who was section chief of emergency medicine and medical director of the emergency department at DHMC at the time. Leaders of similar programs had told him not to expect a call the first day—or even week. But on that hot day in July, the helicopter and its crew completed seven missions.

“It was probably the best day in my career,” Yanofsky says, adding that the program’s immediate success was undeniable proof that the newly minted Dartmouth-Hitchcock Air Response Team (DHART) program was sorely needed. “We’d been working on this for a long time and to see it happen was incredible.”
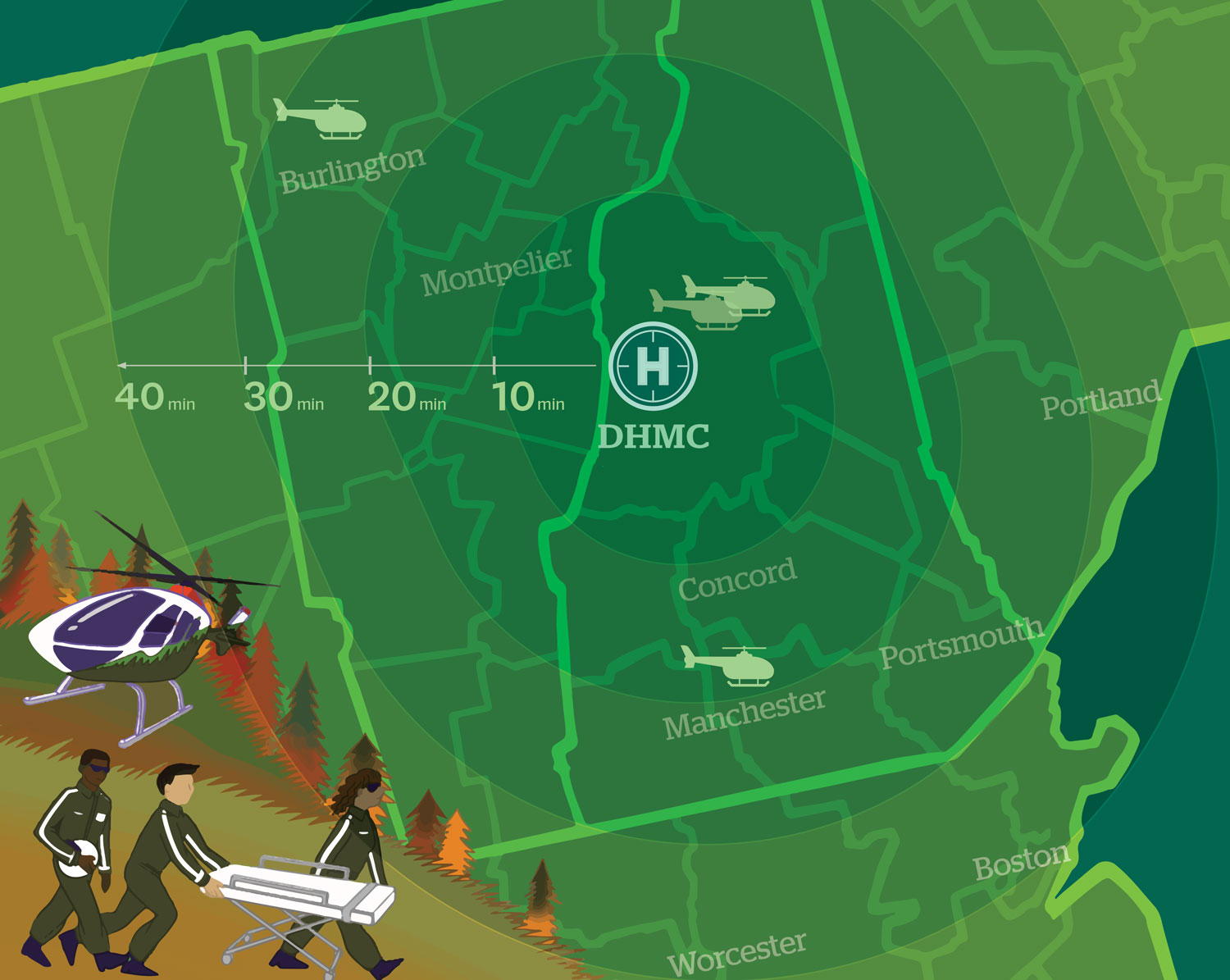
Now, 30 years later, DHART has become an essential component of healthcare in northern New England. The program completes more than 1,500 missions each year and has reshaped how critical care is delivered to the more than 2 million people living in the twin states of New Hampshire and Vermont, as well as neighboring states.
Over the decades, the program’s scope has expanded to include critical care ground transport. Its new name—Dartmouth Health Advanced Response Team—reflects that expansion. Throughout its many chapters, DHART’s mission has remained the same: Provide new ways to ensure that every patient in rural northern New England has access to the highest level of care.
“We changed the way that medicine was delivered,” says John Hinds, a paramedic who has served with DHART since the start, and who retired earlier this year. The crew, he says, has continued to be an innovative powerhouse. “Any challenge that’s been put in front of DHART, DHART has proven it is up to the task.”
With that established foundation and a sterling reputation as lifesavers, DHART is now poised to reimagine medical transport in the region once again, with plans underway to become Dartmouth Health’s solution for all kinds of patient transportation.
Critical Access for Rural Communities
Before DHART came to town, northern New England was one of the only regions in the country without air medical transport. That meant that when someone was injured in a car accident on a hard-to-reach back road, for example, they had to wait—sometimes hours—for paramedics to wind their way through the mountainous, rural terrain on the ground to reach them.
Furthermore, the nearest hospital might have just a handful of emergency room staff, with minimal equipment at their disposal, as many small community hospitals lacked critical care resources (and still do). This meant more travel for the patient, sometimes hours more, to DHMC, which is New Hampshire’s only Level 1 trauma center.
In critical care, delays can be the difference between life and death, says Susan Reeves, EdD, RN, CENP, system chief nursing executive of Dartmouth Health, and a former vice president of emergency services and DHART director. “Before there were ways to rapidly get the most critically ill and injured people to definitive care, they often died,” she says. “Without DHART, we would be losing a lot more lives, plain and simple.”
Northern New England’s rural setting presents more than just a remoteness challenge. Sure, helicopters can land on mountaintops or whiz over river valleys. But that same terrain is often cloaked in clouds, which can make it impossible to fly a helicopter many days of the year.
DHART has solved that issue in two ways, both added to the program in 2001: setting up a nimble ground operation to support air transport, and establishing a system of set routes that could be flown on autopilot in cases of little to no visibility.
These Instrument Flight Rules (IFR) routes are private, so nobody else can use them. They have been scoped out ahead of time to ensure they avoid obstacles, and they are rechecked every two years. DHART director Mike Mulhern estimates that the IFR routes, the establishment of which was supported by philanthropy, have enabled DHART to reach 40 to 50 more patients each year.
The program’s ground vehicles are equipped as advanced life support (ALS) ambulances. These mobile intensive care units (ICUs) provide DHART-level care when a helicopter can’t fly or for interfacility (hospital to hospital) critical care transport when the speed of the helicopter isn’t needed.
DHART has also added two helicopter bases in partnership with Metro Aviation Inc., an aviation operations company that provides pilots, maintenance, and operations management for the program. In 2008, the program added a second base in Manchester, N.H. In 2018, DHART began partnering with the University of Vermont Medical Center to operate a helicopter in Burlington, Vermont. Although DHART primarily covers New Hampshire and Vermont, it also transports patients as far as the Atlantic Ocean in Maine and the Adirondacks in New York, and provides mutual aid in all states bordering Canada to as far south as New York City.
“If you’re going to have an academic medical center in the woods, you need a way to get your patients to you. That’s why the DHART program was born,” Reeves says.
More Than Transporation
DHART saves lives with speedy transportation and by providing vital medical care along the way. Nobody knows this better than Caroline Alley.
In January 2022, Alley suffered from severe hypothermia after getting locked outside in just a bathing suit in frigid Stratton, Vt., after a dip in the hot tub. Within minutes, Alley lost consciousness. When firefighters found her two hours later, her body temperature had dropped to 73 degrees.
The firefighters quickly realized that she needed a hospital; Alley was running out of time. Thankfully, DHART soon arrived. En route to DHMC, where a hyperbaric chamber awaited her, paramedics used blood fluid warmers to treat Alley. She credits this in-air action with saving her life.
“My doctors were shocked I made it,” Alley says. “The DHART team quickly identified the treatment I would need. They were able to start a central line and begin warming my blood, providing me with the critical care I needed until we made it to the hospital. Although my accident led to wounds, skin grafts, and amputated toes, I am able to live my life normally today thanks to their incredible support. They truly are heroes.”

Earlier this year, Alley led a fundraiser for DHART to purchase more advanced blood fluid warmers, one of the many tools DHART paramedics and nurses use in the field.
“We are essentially an extension of the care that you’re getting at Dartmouth Hitchcock Medical Center in the back of an ambulance or helicopter,” Mulhern says, referencing DHART’s ability to perform everything from transfusions to intubations to life-saving cardiac support. “The helicopter is set up for a day’s worth of ICU-level care.”
But it wasn’t always that way. “When we first started, I wouldn’t have put in a chest tube. I would never have cut somebody’s throat to keep them breathing. We didn’t give blood,” says Hinds, the paramedic. Over time, the team was entrusted with more sophisticated trauma interventions and trained to deliver ICU-level care—which gives patients like Alley the critical care they need before they arrive at DHMC.
DHART in Your ER
When DHART began, the program primarily served as transportation from accident scenes and other clinical facilities to DHMC. But as the medical response team expanded the care they provided on the fly, small hospitals across New Hampshire and Vermont increasingly came to see DHART as a resource to call on for more than just transportation.
“The critical access hospitals in our region are often staffed with one to two nurses, and one provider. Resources are really limited,” says Jess Ryan, RN, MSN, CPHQ, system vice president of care coordination for Dartmouth Health. So DHART has filled the gap in urgent situations.
Ryan herself was once one of those nurses, working alone in a five-bed emergency department in Vermont. She recalls a time when a motorcycle accident brought two critical amputation patients in and they were running out of O negative blood. “It was such a relief” when DHART arrived, Ryan says, bringing with them blood supplies and extra, highly skilled hands to stabilize the patients before transporting them to DHMC.
“DHART is a helping hand,” Mulhern says. “We can fly out to wherever you are and initiate that same Dartmouth ICU care in your ER or in the back of your ambulance.”
DHART also has a specialized team at the Intensive Care Nursery (ICN) at the Children’s Hospital at DHMC (CHaD) that extends neonatal intensive care beyond the walls of CHaD, New Hampshire’s only children’s hospital. When infants needing complex care are born in facilities that can’t provide it, and when other children across the region are severely ill or injured, DHART and the ICN team are essential to ensuring that they have access to the urgent, specialized care they need to survive.
The Next 30 Years of Lifesaving Care
Small community hospitals and ambulances are increasingly suffering staffing and resource shortages. Dartmouth Health aims to alleviate that problem by expanding the health system approach and strengthening connections with facilities across the region. To that end, DHART will expand to become the health system’s solution for all kinds of transportation.
“As we build DHART as we know it into a comprehensive transportation system entity, we’re looking at both ends of the spectrum, from the high-need critical care resources that DHART currently provides to the non-acute transfers that we know patients need,” Ryan says.
Currently, DHART focuses on critically injured and ill patients, but there is also a need for transportation that isn’t as urgent: Some patients need help getting home after a hospital stay or simply don’t have a way to get to regular appointments, for example. Under a phased plan supported by a bequest from a grateful patient, Les Haynes, over the next five years DHART will add new ambulances to focus on basic transport, expand the emergency medical team, enhance the critical care transport program, and deepen DHART’s transportation operations in southern New Hampshire and Vermont. The expansion will mirror how Dartmouth Health operates, evolving with the system to integrate existing patient transportation programs at member hospitals and clinics into the DHART program to better facilitate healthcare in northern New England.
“We changed how critical care is delivered in northern New England 30 years ago,” says Mulhern. “And now we’re changing rural healthcare again.”
To learn more about DHART and future plans for the program, contact Matthew Hall at 603-653-0723 or Matthew.R.Hall@hitchcock.org.