Helping Children with PANS
One morning, your child wakes up and seems like a totally different person. He has overwhelming obsessions, aversions, anxieties, and tics. He can’t leave the house and rages at the slightest frustrations. For families who have experienced the disorder known as PANS—pediatric acute-onset neuropsychiatric syndrome—finding the right care is often fraught with long wait times, conflicting diagnoses, and unsuccessful medication trials.

Juliette Madan, MD, MS, a physician-scientist, pediatrician, and psychiatrist at the Children’s Hospital at Dartmouth-Hitchcock (CHaD), has cared for dozens of children with PANS and related conditions, including Charlie Eaton, pictured here. She and her colleagues at CHaD are among a handful of specialized teams nationwide who care for children with brain inflammation and overactive immune responses that can worsen psychiatric symptoms. Both conditions are often seen in kids with autism but can occur in neurotypical kids, too.
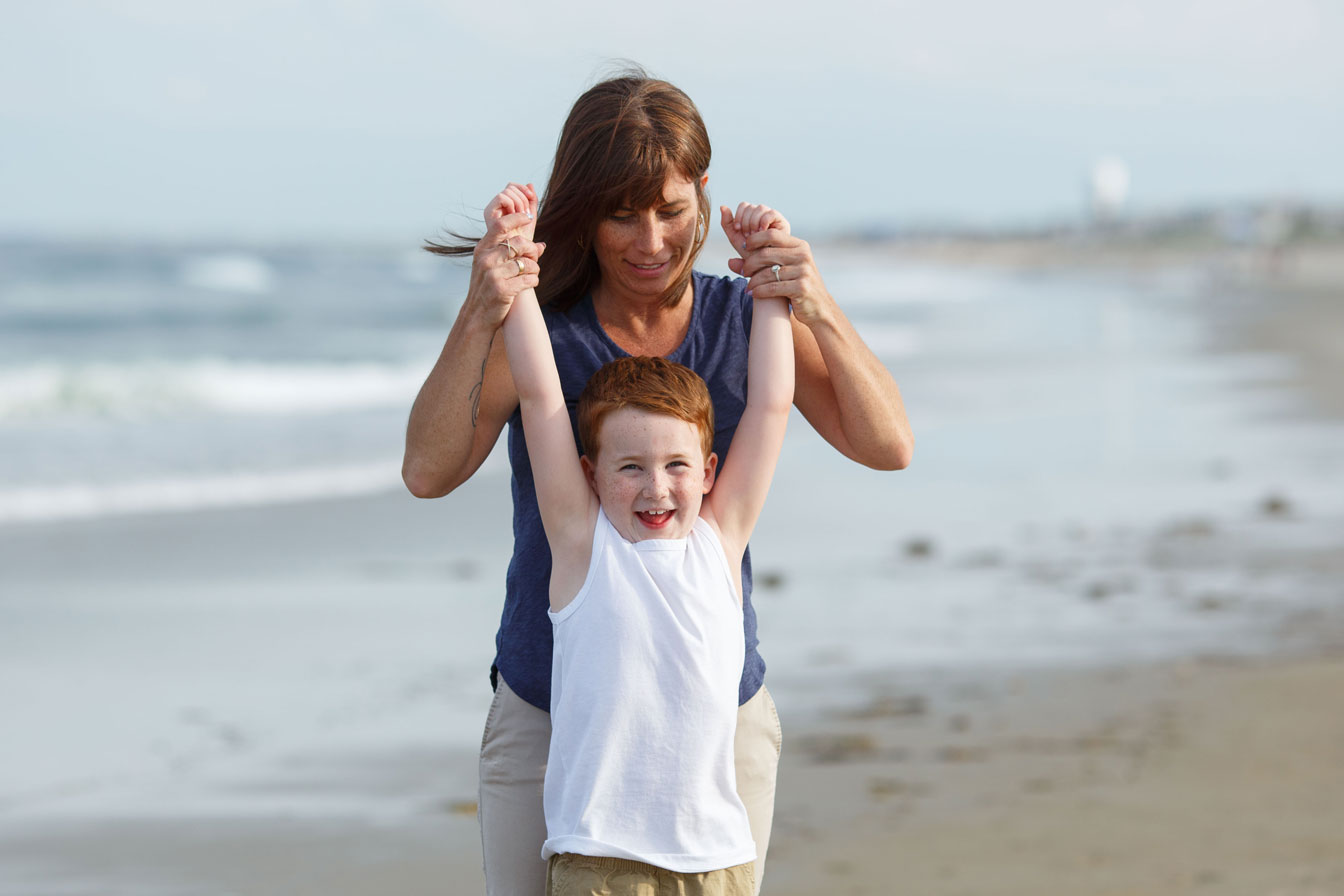
Charlie Eaton was five years old when the severe anxieties and terrifying hallucinations began. By seven, life was unbearable, and his mom was desperate for help. Then, a doctor in Boston confirmed that Charlie had a form of pediatric acute-onset neuropsychiatric syndrome (PANS) and referred them to a highly specialized team at the Children’s Hospital at Dartmouth-Hitchcock. Under their care, Charlie has finally gotten the help he needs. The hallucinations are gone, the anxieties are lessening, and Charlie is back to enjoying life, including going to the beach in their hometown of Seabrook, New Hampshire. Photo by Mark Washburn
Hope through PING
In 2019, Madan teamed up with pediatric neurologist Richard Morse, MD, and colleagues in rheumatology and immunology to create the Psychiatry Immunology Neurology Group (PING) within Dartmouth-Hitchcock and CHaD. The PING clinic helps children whose psychiatric symptoms may be related to inflammation in the brain that was triggered by an infection, such as streptococcal pharyngitis, mycoplasma pneumonia, or, more recently, COVID-19.
Each specialist contributes their expertise and recommendations to help these children. Often a child’s worst symptoms disappear within days of receiving the right treatment. Within months, many children are symptom free and working with therapists to move past any lingering anxieties.
“We must open our minds to the possibility that some children with severe behavioral and psychiatric syndromes have an underlying immune, infectious, or inflammatory process,” explains Madan. “A very small percentage of children have such conditions, probably less than 1% of all children, but for these patients and their families, the impact is enormous and requires a multi-pronged approach.”
Investigating the gut-brain connection
Finding the underlying cause of diseases in children has been Madan’s passion for more than a decade. An associate professor of pediatrics and epidemiology and faculty member of the quantitative biomedical sciences graduate program at the Geisel School of Medicine at Dartmouth, Madan is the longtime clinical director of research for Geisel’s Children’s Environmental Health and Disease Prevention Research Center (“Children’s Center”), a top fundraising priority for the school. In that role, she helps direct the New Hampshire Birth Cohort Study, which collects health data and biological samples from over 2,000 pregnant women and their children at key developmental points in infancy and early childhood.
One day, we hope to leverage the power of the gut microbiome and other interventions to truly heal these children, and, ultimately, help them live their happiest, healthiest lives.”
—Juliette Madan, MD, MS
As part of the Children’s Center, Madan’s research team studies the early life microbiome: the ecosystem of microscopic organisms that inhabit our skin, digestive tract, and many other organs. In the gut, the microbiome helps regulate digestion, train the immune system, and drive neurodevelopment, which then affects emotions and behaviors. This makes it a prime location to study and potentially heal behavioral, neurological, and immune disorders—including PANS, autism, anxiety, and inattention.
The autism community has long embraced the gut-brain connection and the possibility that dysregulated immune systems contribute to autistic behaviors. Consider that children with autism have high rates of allergies, asthma, anxiety, ADHD, and digestive disorders.
“The patterns that we identify in the microbiome and that relate to disease can be altered,” explains Madan, “giving us tremendous hope for prevention and treating disease.” A recent study from Madan’s lab has shown that children who exhibit autism-related behaviors by age 3 have unusual populations of microorganisms in the gut. More research and funding is needed to determine targets for treatment.
Gifts to Power Research and Care
In the next year, Madan hopes to attract philanthropic and grant funding to support several clinical studies aimed at developing interventions—such as fecal transplants and probiotics—that could help children with PANS, autism, or other related illnesses.
Recently, the PACE Foundation has facilitated funding in support of PANS care at Dartmouth-Hitchcock and its participation in a national network of academic medical centers that collaborate to study and treat pediatric autoimmune neurological disorders. PACE is also arranging funding for a microbiome study of children with PANS, with the chief collaborators being researchers at Geisel’s Children’s Center and the University of Arizona.
“One day, we hope to leverage the power of the gut microbiome and other interventions to truly heal these children, and, ultimately, help them live their happiest, healthiest lives,” Madan says.
(Families who think their child may benefit from a PING consult should talk first with their primary care doctor and/or mental health provider, if they have one.)