AI at the Cutting Edge of Surgery
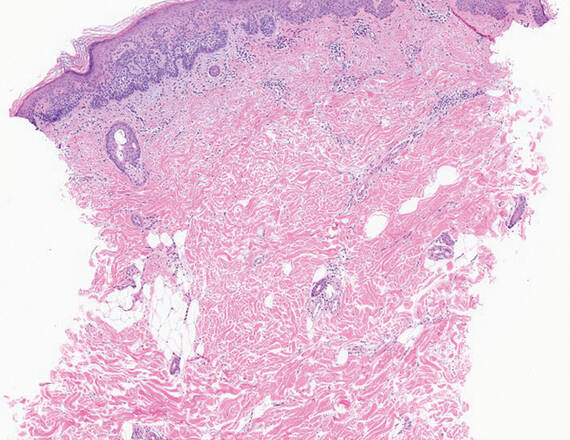
Surgeons face a delicate balance when removing a cancerous tumor: They need to extract all of the cancer while leaving as much healthy tissue intact as possible.
But figuring out exactly where that line lies can be tricky. So Matt LeBoeuf, MD, PhD, section chief and director of Mohs Micrographic Surgery in the Department of Dermatology at Dartmouth Hitchcock Medical Center and the Geisel School of Medicine at Dartmouth, and his colleagues are investigating how artificial intelligence (AI) and machine learning could help surgeons make the most precise excisions possible in real time.

Most surgeries require removing the tumor and sending the tissue to a lab for analysis of the margins, which could take days and can delay fixing the site. The dilemma lies in the question of how much tissue to remove—the larger the margin, the better the chance that all the cancer is removed, but it’s also more likely that too much healthy tissue goes with it. On the other hand, if the margin is too small, some cancerous tissue might remain, resulting in the need for another surgery.
Currently, even without AI, LeBoeuf can make these kinds of decisions in real time during surgery, but this approach is largely limited to skin cancers treated within the Dermatology Department at Dartmouth Hitchcock Medical Center (DHMC). That’s because there’s a pathology lab onsite and LeBoeuf has specialty training to analyze and precisely map any remaining tumor—but not all surgeons have that training. Typically, LeBoeuf uses a 1- to 2-millimeter margin of tissue during surgery, and then analyzes the margin within 15 to 30 minutes. He can easily return to surgery and excise more tissue if needed.
“It’s an iterative process of removing tumors, and doing it this way results in less than 0.5% recurrence,” LeBoeuf says. It also helps him spare surrounding healthy tissue. With confidence that the tumor is completely removed, he can fix the surgical site the same day. LeBoeuf wants to make this procedure seamless in other departments at DHMC and at other institutions, and one way of making that possible, he says, is using AI.
In his research, LeBoeuf is working to use AI to combine the logistical processes of analyzing tissue. “AI takes all of these skillsets and puts them into one virtual platform, which automates these decisions,” he says. No longer would a pathologist have to be onsite for real-time analysis—they could analyze the tissue digitally from anywhere in the world.
“We’ve started thinking about how this can be applied to non-skin cancers, too, specifically oral and airway cancers,” LeBoeuf says. “Those types of tumors have high rates of positive margins and the tumor coming back.”
Yet, particularly with oral and airway cancers, excising more tissue might mean that surrounding anatomic structures are affected, maybe unnecessarily. AI could help minimize this possibility all over the body.
“This has a great potential to change the way we do surgery in the future, and we’re moving forward in a thoughtful, deliberate manner,” says LeBoeuf, who is collaborating with others, including Louis Vaickus, MD, PhD, medical director of pathology informatics at DHMC, and Joshua Levy, PhD ’21, assistant professor of dermatology at the Geisel School of Medicine at Dartmouth. LeBoeuf notes, “We must be skeptical of anything that’s new. With AI, you’re assuming the computer will do the job as well as human surgeons do currently, and that’s a lot to ask right now. We must make sure patients are protected.”
Although this technology won’t be ready for implementation for many years, LeBoeuf says the AI algorithm already is highly effective at detecting and mapping tumors; however, the research so far has focused on only one tumor type and only at DHMC. LeBoeuf says the algorithm will need to be adjusted for other types of tumors and different analysis equipment at other clinics.
“The biggest challenge with AI is ensuring the algorithms used with internal data can be applied to external data, such as slides from other medical centers. Slide variations make a big difference with algorithms,” LeBoeuf says. “This is a reasonable next step for future grant funding; we would do multi-institutional collaborations. The algorithm is performing extremely well here, and we want to make sure it can be broadly applied anywhere in the country and hopefully even beyond.”