Nationwide, patients are languishing on waiting lists. This department devised a solution.
In just a single week, the Department of Dermatology cleared almost its entire waiting list of nearly 4,000 patients, some of whom had been longing to get an appointment for months. The schedules-cleared, all-hands-on-deck approach to improving new patient access—aptly named Patient Access Week—was the first of its kind in the nation.

The problem of unwieldy waiting lists isn’t exclusive to Dartmouth Health: Dermatology clinics across the country are experiencing huge referral backlogs, particularly in academic medical centers. Among the many contributing reasons is the concern that physicians will not have enough appointments available for established patients who need follow-up care. In addition, academic medical centers typically have a smaller number of dermatologists on staff but receive referrals from outside clinics to handle more complex presentations. For certain conditions, patients might have to wait six months for an appointment simply because there are fewer subspecialty providers.
Shane Chapman, MD, MBA, RES ’99, chair of the Department of Dermatology at Dartmouth Hitchcock Medical Center and the Geisel School of Medicine at Dartmouth, couldn’t accept that these patients had to wait so long for the care they needed. So, Chapman; Caitlin Yazel, APRN, Dermatology nurse manager; and other department leadership worked to create a plan to solve the backlog, which they first implemented December 11-15, 2023.
The Countdown Begins
“Shane had the idea for a new patient access week, and we started planning in April 2023,” Yazel says. “We pulled our thoughts together to consider all the potential problems, like how would patients move through the clinic? And are we going to have enough space in the parking lot?”
With so many patients to see, the entire department, including physicians, nurses, medical assistants, residents, administrative assistants, the research team—literally everyone—came to clinic all day every day. As a testament to the thoughtful planning, no one in the Department of Dermatology called in sick or took vacation that week.
“A key cultural point was asking faculty regularly for their input,” Yazel says. “We gave updates at faculty meetings and asked, ‘What makes you nervous about this? What aren’t we thinking of?’”
Yazel also brought the plan to the nursing team for input. Everyone brought up different potential obstacles, so by the time the big week arrived, nearly all the kinks had been worked out. “That was our strategy to address concerns that might make this plan unsuccessful,” she says. “People had opportunities to think this through.”
Making the Most of Every Appointment
Among the concerns were logistics—getting so many patients in the door for appointments would not be easy. To make it happen, visits were limited to about 10 to 15 minutes to discuss the patient’s main concern. If a patient had a complex issue, Chapman or Yazel would handle the case, so the faculty could keep the flow of patients moving smoothly.
Cheyanne Jones, RN, felt apprehensive about how to handle the sheer volume of patients. The answer was to change the normal appointment model.
“We weren’t on a specific provider schedule. It was more like first come, first served,” Jones says. “There were a certain number of patients scheduled at 9:00 am, a certain number at 10:00 am, and so on. Whichever provider was ready for another patient would come out to get someone.”
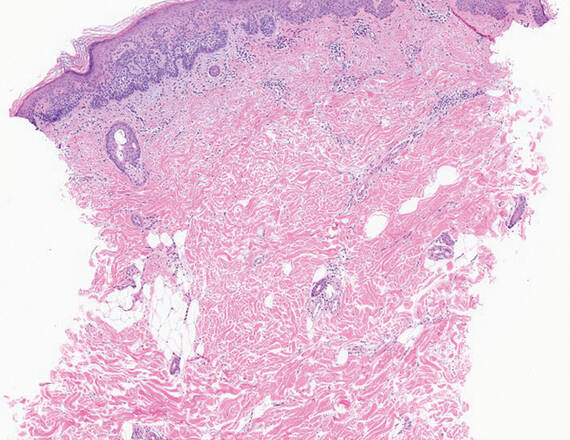
Julianne Mann, MD, MED ’07, section chief of Pediatric Dermatology, says it felt exhilarating to serve so many patients that week. She recalled one of her patients who had a large melanoma on the back. “It’s so rewarding to see someone like that patient and think, ‘Wow, if this melanoma had progressed, this patient’s journey could have been very different.’
“We chose medicine as a profession because we want to make a difference in people’s lives. One way to do that is to create access for patients who are waiting to be seen,” Mann says. “With this new model, we can reach patients who need us. That’s very rewarding and makes the extra effort well worth it.”
Residents in the Mix
Residents also contributed to the week’s success, forgoing surgeries and didactic learning in order to spend all their time in clinic. In addition to the positive feeling of helping so many patients, residents also enjoyed the sense of teamwork.
“It was cool to come together as a team and see all the energy throughout the week,” says Matthew Davis, MD, a fourth-year resident. “We all had the same mindset and same goal of seeing as many new patients as possible. It was a lot of work, but a great solution to a complex problem.”
“We were tired but satisfied,” says Dylan Badin, MD, a third-year resident. “We’ve been through a tough challenge together. As residents, we’ve been studying it, and now we can see it, diagnose it, and treat it. The things we’ve been learning correlates with good patient care.
A Model for Success
The department held more patient access weeks in February, April, and June. Most of these were follow-up appointments, and since then, the department’s schedules have returned to normal. The fears that faculty might become overwhelmed with new patient follow-ups, thankfully, didn’t come to bear.
Even though appointments were brief, the high ratings on the department’s patient survey revealed that patients were pleased with their care and appreciated that providers took time to connect with them on a personal level.
Newport, Vermont, residents Daniel Cordeau and Ann Azur-Cordeau were among the patients seen in April—though only Ann had an appointment. But Daniel had recently been referred to a dermatologist for a concerning spot on his back and wondered whether Brian Simmons, MD, RES ’20, would mind taking a look after he finished with Ann’s examination.
“I just mentioned it to him; I didn’t think he’d do anything. But he looked at it and said, ‘We can take care of that,’” says Dan, who had the concerning spot removed the same day, thanks to a cancelation in Simmons’ schedule. “I’ve never been in a hospital like this where a doctor will say, ‘I’ll do it now.’”
Yazel, Jones, the residents, and others all said the model was a huge success and that it could be applied to other departments dealing with patient backlogs. “It might look different because patient needs in other departments are different,” Yazel says, “but the concept can be applied across the spectrum.”